Zanu PF deploys FAZ for by-elections
Local News
By Problem Masau
| 17h ago
Our roads a nightmare: Mohadi
By Mthandazo Nyoni
17h ago
.
Videos
Pamela Marwisa In Conversation With Trevor
By The NewsDay
Feb. 28, 2024
By The NewsDay
Feb. 28, 2024
By The NewsDay
Dec. 5, 2023
Old Mutual launches funeral services in Masvingo
Sponsored Content
Vintage travel and tours reveals its successes
Sponsored Content
EcoCash extends payroll services to security companies
Sponsored Content
Stanbic Bank opens more branches for tobacco players
Muhau said the setting up of three more implants was one way of living up to that commitment as it brings banking facilities closer to the regions of production.
By Agriculture Reporter
Apr. 25, 2024
Study rules out human factor in southern Africa drought
By Nhau Mangirazi
Apr. 20, 2024
El Niño to trigger drought insurance payouts in Zimbabwe
By Bloomberg News
Apr. 19, 2024
Demand for milk seen softening
By Mthandazo Nyoni
Apr. 18, 2024
Govt sets target for winter wheat production
By Priviledge Gumbodete
Apr. 17, 2024
Govt to clamp down on cotton side marketers
By Blessed Ndlovu
Apr. 11, 2024
High rabbit pellets prices choke Zimbabwe farmers
By Mthandazo Nyoni
Apr. 5, 2024
Tobacco firm BAT hires new MD
By Blessed Ndlovu
Apr. 4, 2024
Pussyfooting around over ZiG deadly
By Newsday
Apr. 24, 2024
Let’s walk the talk on grain reserves
By Newsday
Apr. 23, 2024
Confidence is earned, indeed!
By Newsday
Apr. 22, 2024
Professionalism key in luring sponsors
By admin
Apr. 20, 2024
Economy, drought cast pall on Uhuru celebrations
By Newsday
Apr. 19, 2024
Interest rates seen tumbling below 20%
By Mthandazo Nyoni
Apr. 25, 2024
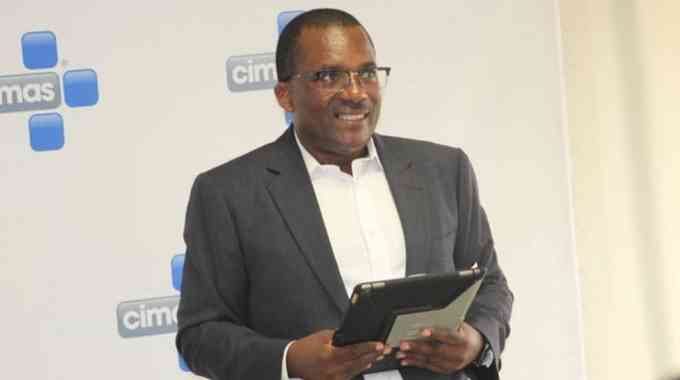
Nyazema lands CBZ CEO post
By Blessed Ndlovu
Apr. 25, 2024
Invictus inks gas to power deal
By TAFADZWA MHLANGA
Apr. 24, 2024
CBZ appoints Zembe chairperson
By Blessed Ndlovu
Apr. 24, 2024
Zimplow CEO resigns
By Business Reporter
Apr. 24, 2024
Zim exports uncompetitive: ZimTrade
By Melody Chikono
Apr. 24, 2024
.
Sport
.
Opinion
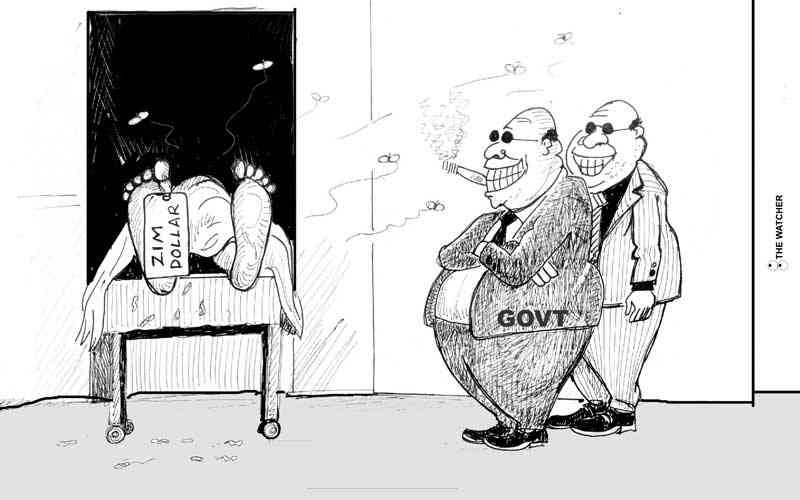
NewsDay cartoon 28 November, 2023 edition
NewsDay cartoon 28 November, 2023 edition
By The Watcher
Nov. 28, 2023
Govt urges unity among lithium miners
Currently there are around eight different lithium exploration and mining projects at different development stages.
By Mthandazo Nyoni
Jun. 1, 2023
Over 130 civilians killed by DR Congo rebels - UN
By BBC News
Dec. 8, 2022
Opaque Chinese deals: Mthuli taken to task
By admin
Aug. 29, 2022
Power outages, raw material shortages hit ART operations
By The NewsDay
Aug. 17, 2022
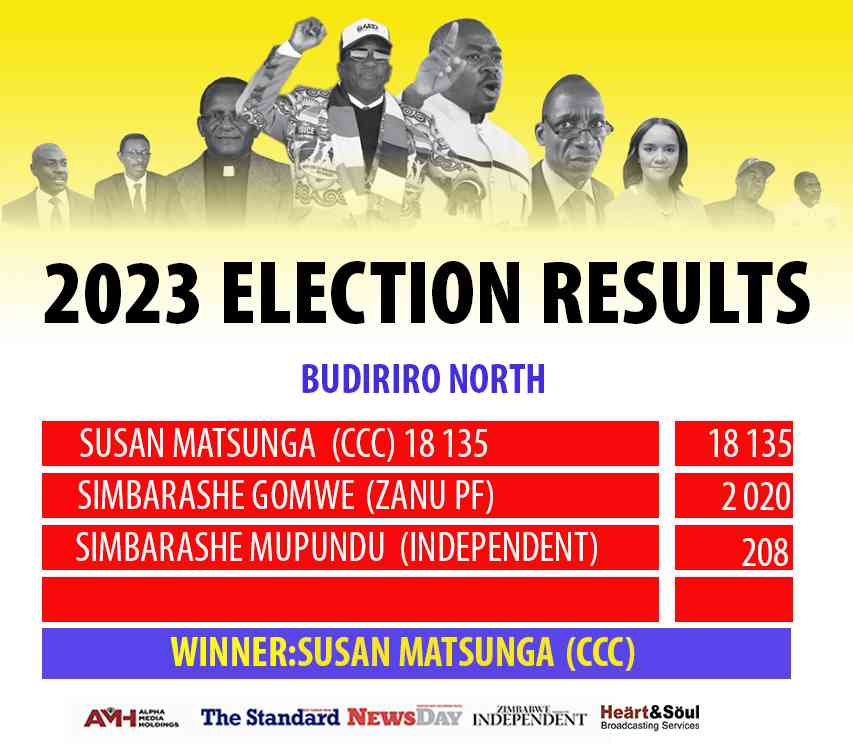
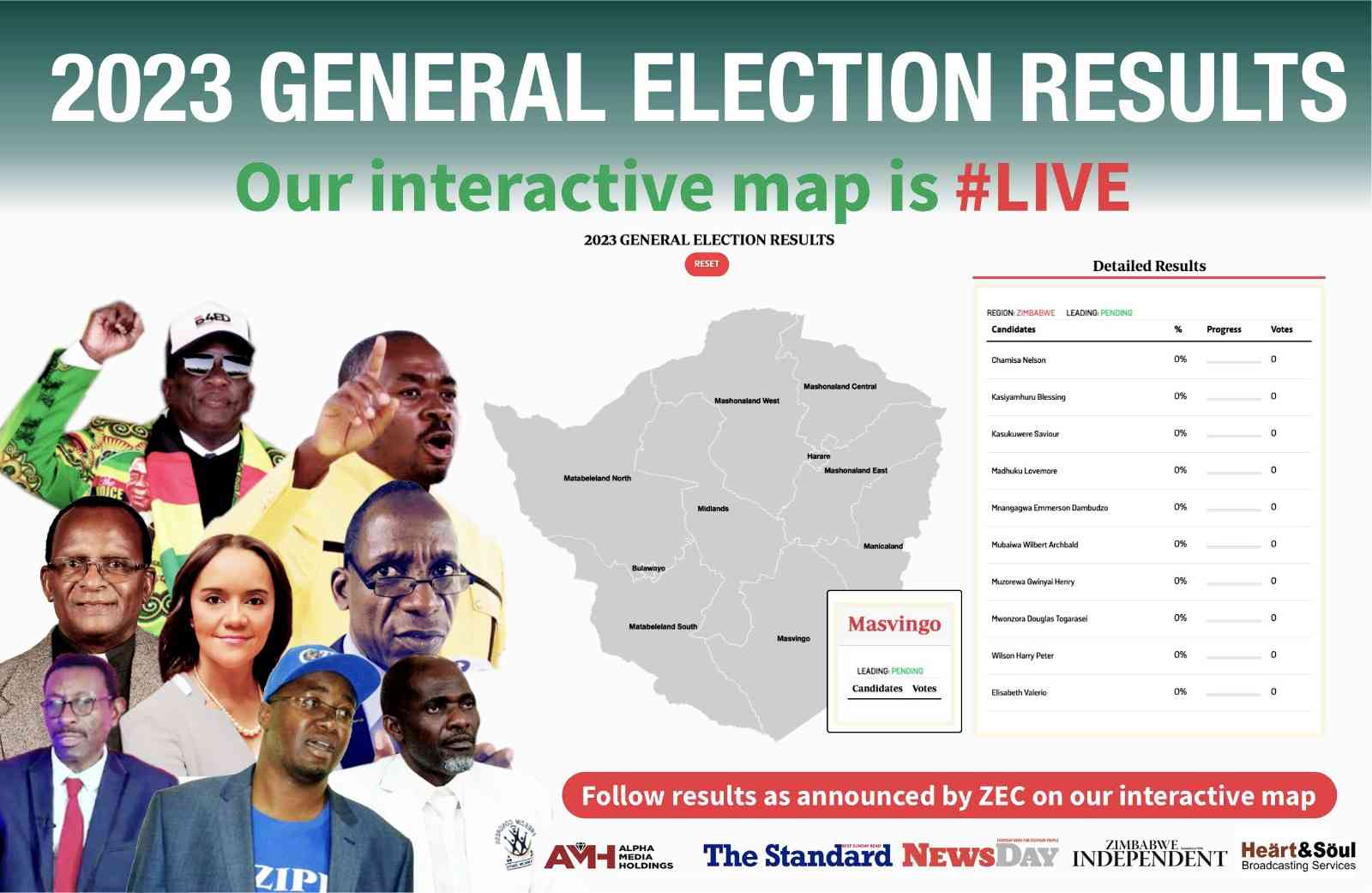
We’re unstoppable: CCC
By The NewsDay
Aug. 16, 2022
Umzingwane, Matobo main road ‘forgotten’
Matobo ward 15 councillor Dickson Moyo said the Old Gwanda road, which is major road passing through Umzingane and Matobo, had been neglected for more than five years.
By The NewsDay
Jul. 29, 2022
The existential crisis of Zim’s national identity
Throughout our rich history, we have fought against colonialism, struggled for independence, and yearned for a future defined by justice and equality.
By AMH Voices
Apr. 25, 2024
Prophet lauds Tanzania, Zimbabwe relationship
Madzibaba Jonah usually goes around the continent and Asian countries where he joins other apostolic members in prayer.
By Style Reporter
Apr. 25, 2024
Wash boost for indigenous churches
By Style Reporter
Apr. 24, 2024
Mahachi pays tribute to late SA gospel icon
By Style Reporter
Apr. 23, 2024
Richest Forex Traders in Tanzania
By The Standard
Apr. 22, 2024
Gwanda water crisis deepens
“Efforts to sink deeper the pipe that draws water are being made, but this is not a final solution, it's just a short term measure as we wait for Zinwa to bring water from Blanket Dam.”
By Silas Nkala
17h ago
We’ll be Zim’s industrial hub again: Coltart
By Silas Nkala
Apr. 25, 2024
Binga South MP, minister clash over boreholes
By Patricia Sibanda
Apr. 25, 2024
Premium
Zim secures multi-million dollar jet deal

Mushshak is an Urdu (official Pakistan national language) word which translates to proficient.
By Tinashe Kairiza
11h ago