BY VENERANDA LANGA
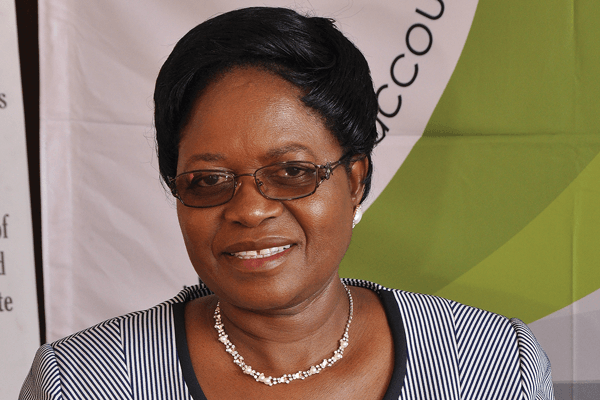
AUDITOR-GENERAL (AG) Mildred Chiri says analysis of maternal mortality statistics indicate that maternal deaths in Zimbabwe were still high, although they had gone down from 790 deaths per year in 2013 to 522 in 2016.
Chiri said this in her audit report on the management of maternal healthcare by the Ministry of Health and Child Care, which was tabled in the National Assembly on Thursday by deputy Speaker Tsitsi Gezi.
The AG said although the statistics presented to her by the Ministry of Health were not reliable, the information on the statistics came from demographic surveys conducted by the Zimbabwe National Statistical Agency (ZimStats) done every five years, which showed that maternal mortality ratio had declined from 960 deaths per 100 000 live births in 2009 to 651 per 100 000 live births in 2015.
“The statistics presented by the ministry were, therefore, being understated as deaths that took place in private health facilities were not included,” Chiri said.
“According to 2014 and 2015 maternal death annual reports and 2015 Reproductive Health annual report, the Ministry of Health was facing challenges with Health Management Information Systems (HMIS) in the provision of timely, reliable and accessible health information, including maternal mortality data,” she said.
The AG said besides the non-reporting of maternal health from private health facilities, review of Manicaland’s annual reports indicated that maternal mortality statistics presented by the ministry were also being understated as deaths that took place in some communities were not being reported.
“According to the reports, maternal health statistics by village health workers in some communities were poorly prepared, untimely and unreliable. Interviews with village health workers at two of the facilities visited in Nyanga district revealed that they faced a lot of challenges in conducting their activities and this was affecting collection and assembling of data.”
- Chamisa under fire over US$120K donation
- Mavhunga puts DeMbare into Chibuku quarterfinals
- Pension funds bet on Cabora Bassa oilfields
- Councils defy govt fire tender directive
Keep Reading
Chiri said the response by the Health ministry was that institutional maternal deaths measured yearly were reduced from 1 200 deaths in 2010 to 525 deaths in 2015, but this was also below the targets set by the Ministry of Health.
“The ministry acknowledged that there were maternal deaths which occur in communities and might not have been reported. This calls for the strengthening and increasing of the numbers of community health workers and improvements in their training,” she said.
The AG also said the other problem was that a considerable proportion of pregnant women either registered their pregnancies late or failed to register the pregnancies at all.
She said some of the major causes of maternal mortality were unaffordable maternity costs and inaccessibility of primary maternal health facilities.
“Although the ministry stated that pregnant women should obtain maternal health care for free, it was established that some health facilities were still levying maternity fees. Audit noted that 29% of the 35 health facilities visited were levying maternity registration fees ranging from $25 to $30, and these facilities were primary health facilities in urban councils,” she said.
Chiri also said some pregnant women in urban councils travelled 25km seeking maternal healthcare, while those in remote rural areas were more vulnerable as they had to travel in, some instances, more than 40km.











