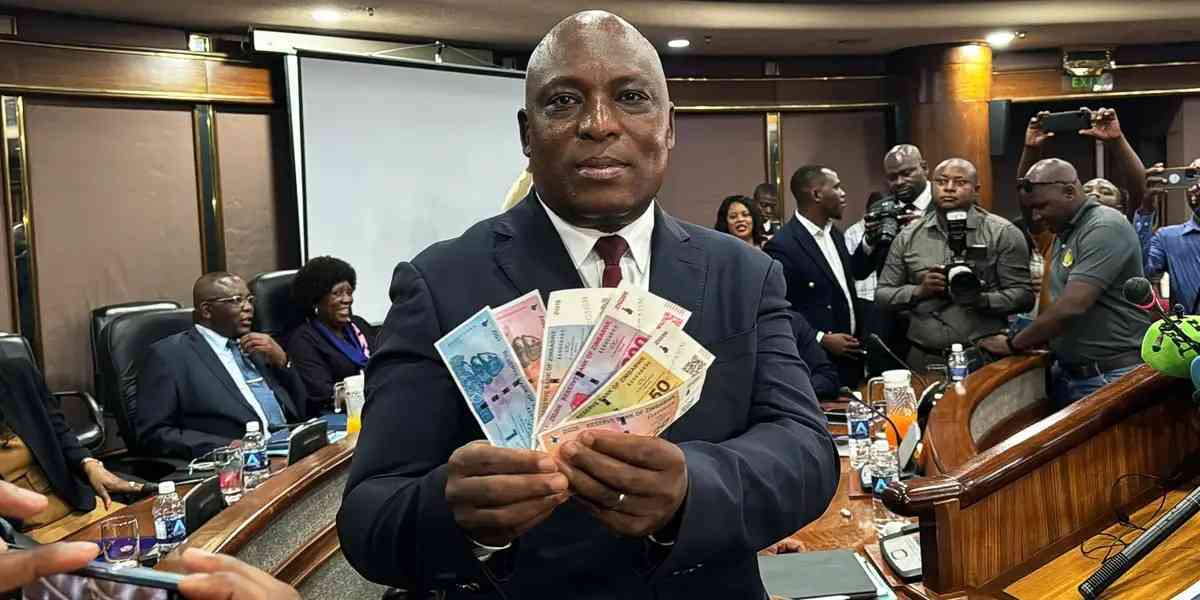
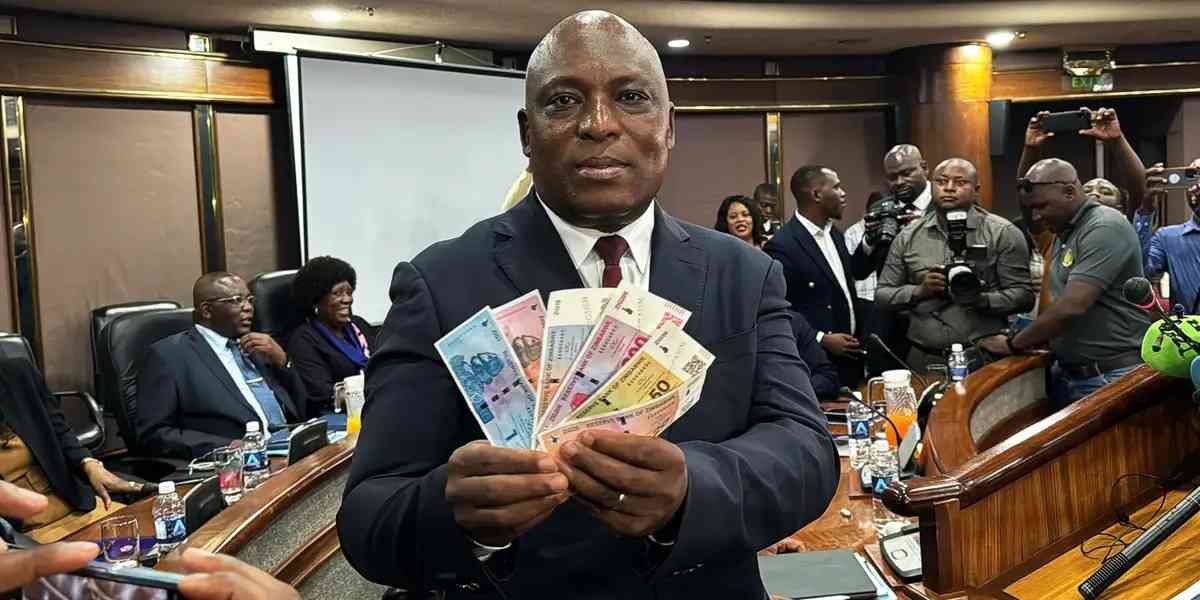
I’ll report back if ZiG fails: RBZ governor
Local News
By Nizbert Moyo
| Apr. 18, 2024
I’ll report back if ZiG fails: RBZ governor
By Nizbert Moyo
Apr. 18, 2024
BCC redesigns vending bays at Egodini
By Innocent Magondo
Apr. 18, 2024
‘Guard against weaponisation of food aid’
By Harriet Chikandiwa
Apr. 18, 2024
Tighten laws to control internet: Potraz
By BRENT SHAMU
Apr. 18, 2024
Sikhala to speak at global human rights summit
By Staff Reporter
Apr. 18, 2024
Ex-Zacc commissioner trial fails to kick-off
By TREVOR MUTSVAIRO
Apr. 18, 2024
.
Videos
Pamela Marwisa In Conversation With Trevor
By The NewsDay
Feb. 28, 2024
By The NewsDay
Feb. 28, 2024
By The NewsDay
Dec. 5, 2023
Old Mutual launches funeral services in Masvingo
Sponsored Content
Vintage travel and tours reveals its successes
Sponsored Content
EcoCash extends payroll services to security companies
Sponsored Content
Demand for milk seen softening
Morgan & Co estimated a FY24 price target of US$0,0943 that is largely driven by an enterprise value to its earnings before interest, taxes, depreciation and amortisation valuation.
By Mthandazo Nyoni
Apr. 18, 2024
Govt sets target for winter wheat production
By Priviledge Gumbodete
Apr. 17, 2024
El Niño drives Zimbabwean millers to seek Brazilian corn
By Bloomberg News
Apr. 16, 2024
Govt to clamp down on cotton side marketers
By Blessed Ndlovu
Apr. 11, 2024
High rabbit pellets prices choke Zimbabwe farmers
By Mthandazo Nyoni
Apr. 5, 2024
Govt sets target for winter wheat cropping
By Harriet Chikandiwa
Mar. 30, 2024
Smart farming to fight El Nino
By Nhau Mangirazi
Mar. 30, 2024
CIMMYT develops multiple stress tolerant maize varieties
By Mthandazo Nyoni
Mar. 28, 2024
Bullying tactics will not work
By Newsday
Apr. 16, 2024
ZiG: Guard against political interference
By Newsday
Apr. 15, 2024
Availability will stabilise sugar prices
By Newsday
Apr. 13, 2024
Moral suasion key for currency survival
By Newsday
Apr. 12, 2024
Kwibuka 30: Lessons for Zim
By Newsday
Apr. 11, 2024
ZRA repackages Batoka Gorge project

The project scope includes construction of the dam wall for US$1,4 billion, power station at US$1,3 billion and other aspects giving a total of US$4,5 billion.
By TAFADZWA MHLANGA
Apr. 18, 2024
Shot in the arm for the Deeds Registry
By Business Reporter
Apr. 18, 2024
Mind your pricing regime, HAZ warns operators
By Freeman Makopa
Apr. 17, 2024
Access to credit by women improves
By Mthandazo Nyoni
Apr. 17, 2024
It won’t be business as usual, RBZ boss tells staff
By Mthandazo Nyoni
Apr. 17, 2024
Premier seeks US$3,74 million for Zulu project
By Mthandazo Nyoni
Apr. 16, 2024
Firm order book boosts Masimba revenue
By BELINDA CHIROODZA
Apr. 16, 2024
Datvest records ZWL$255,2 million profit
By TAFADZWA MHLANGA
Apr. 16, 2024
Depressed ZSE activity looms
By Mthandazo Nyoni
Apr. 16, 2024
.
Sport
.
Opinion
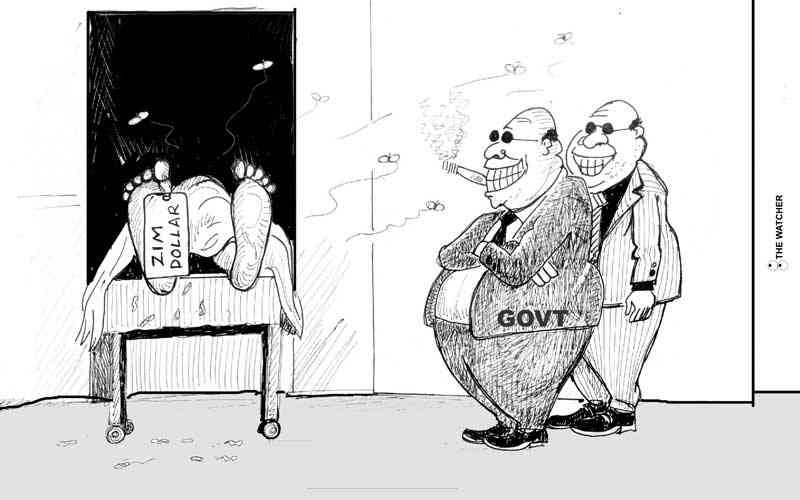
NewsDay cartoon 28 November, 2023 edition
NewsDay cartoon 28 November, 2023 edition
By The Watcher
Nov. 28, 2023
Govt urges unity among lithium miners
Currently there are around eight different lithium exploration and mining projects at different development stages.
By Mthandazo Nyoni
Jun. 1, 2023
Over 130 civilians killed by DR Congo rebels - UN
By BBC News
Dec. 8, 2022
Opaque Chinese deals: Mthuli taken to task
By admin
Aug. 29, 2022
Power outages, raw material shortages hit ART operations
By The NewsDay
Aug. 17, 2022
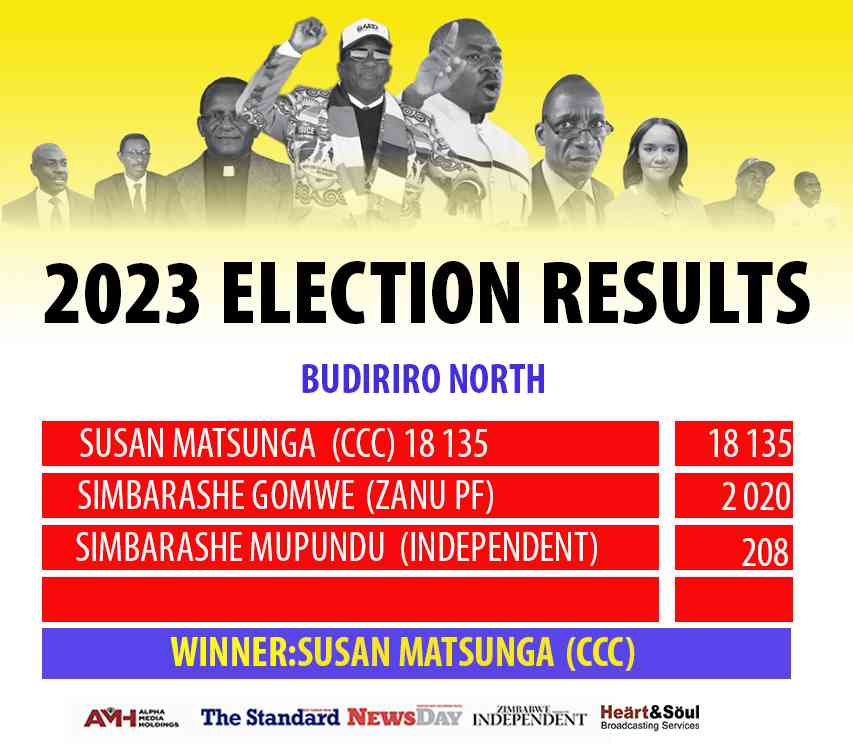
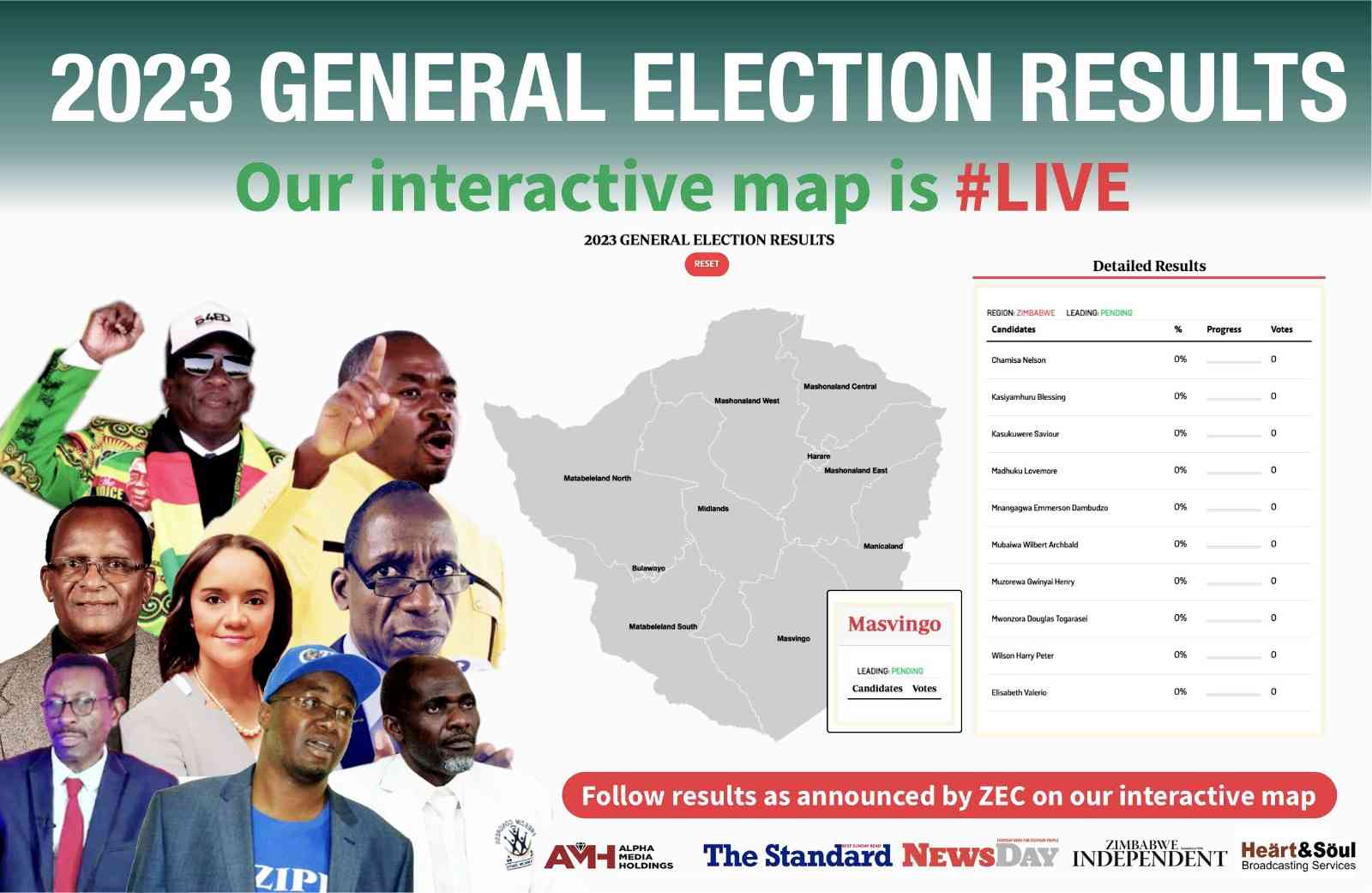
We’re unstoppable: CCC
By The NewsDay
Aug. 16, 2022
Umzingwane, Matobo main road ‘forgotten’
Matobo ward 15 councillor Dickson Moyo said the Old Gwanda road, which is major road passing through Umzingane and Matobo, had been neglected for more than five years.
By The NewsDay
Jul. 29, 2022
Diasporas must vote in Zim elections

The Zimbabwe Diaspora Vote Initiative closely followed the Russian elections, monitoring how the Russian government handled diaspora voting in that election.
By AMH Voices
Apr. 6, 2024
Lady Chevrons vie for World Cup place
By AUSTIN KARONGA
Apr. 14, 2024
Youth move in to get slice of construction industry cake
Chihota gave thumbs up to the parent association, ZBCA, for coming up with such an initiative.
By Staff Reporter
Apr. 14, 2024
Makarati boost for DeMbare
By Henry Mhara
Apr. 14, 2024
Scores arrested for booing Auxillia
By KUMBIRAI MAFUNDA and Everson Mushava
Apr. 14, 2024
Champions Ngezi Platinum snatch point from Bosso
By Munyaradzi Madzokere
Apr. 14, 2024
Govt fails to pay civil servants for blitz
By Miriam Mangwaya
Apr. 14, 2024
Overflowing toilets a health time bomb
By JERSSIE MPOFU
Apr. 18, 2024
NGO mobilises sanitary wear for women in prison, girls
Garura said the initiative would see young girls attending school and avoiding missing classes due to lack of food and sanitary wear.
By Patricia Sibanda
Apr. 18, 2024
Women dominate vending in Bulawayo: Report
By Innocent Magondo
Apr. 18, 2024
Byo humanitarian honoured in Africa
By MARGARET LUBINDA
Apr. 17, 2024
Valve vandalism worsens Bulawayo water crisis
By Innocent Magondo
Apr. 17, 2024
Residents ramp up fight against drug abuse
By Patricia Sibanda
Apr. 17, 2024
Forex Brokers with 1 USD Minimum Deposit in Tanzania

In terms of trading accounts, there are four different accounts that traders can choose from. These include the standard account, the micro account
By Theindependent
Apr. 13, 2024
By Cynthia Tapera
Apr. 12, 2024