Shops face closure over ZiG
Local News
By Mthandazo Nyoni
| 1h ago

Officially opening the international business conference at the Zimbabwe International Trade Fair (ZITF) in Bulawayo, Chiwenga said ZiG was here to stay.
Blackouts spoil ZITF
By Innocent Magondo
2h ago
ED in mini-Cabinet reshuffle
By Staff Reporter
2h ago
.
Videos
Pamela Marwisa In Conversation With Trevor
By The NewsDay
Feb. 28, 2024
By The NewsDay
Feb. 28, 2024
By The NewsDay
Dec. 5, 2023
Old Mutual launches funeral services in Masvingo
Sponsored Content
Vintage travel and tours reveals its successes
Sponsored Content
EcoCash extends payroll services to security companies
Sponsored Content
Stanbic Bank opens more branches for tobacco players
Muhau said the setting up of three more implants was one way of living up to that commitment as it brings banking facilities closer to the regions of production.
By Agriculture Reporter
2h ago
Study rules out human factor in southern Africa drought
By Nhau Mangirazi
Apr. 20, 2024
El Niño to trigger drought insurance payouts in Zimbabwe
By Bloomberg News
Apr. 19, 2024
Demand for milk seen softening
By Mthandazo Nyoni
Apr. 18, 2024
Govt sets target for winter wheat production
By Priviledge Gumbodete
Apr. 17, 2024
Govt to clamp down on cotton side marketers
By Blessed Ndlovu
Apr. 11, 2024
High rabbit pellets prices choke Zimbabwe farmers
By Mthandazo Nyoni
Apr. 5, 2024
Tobacco firm BAT hires new MD
By Blessed Ndlovu
Apr. 4, 2024
Let’s walk the talk on grain reserves
By Newsday
Apr. 23, 2024
Confidence is earned, indeed!
By Newsday
Apr. 22, 2024
Professionalism key in luring sponsors
By admin
Apr. 20, 2024
Economy, drought cast pall on Uhuru celebrations
By Newsday
Apr. 19, 2024
Uhuru at 44: Still a long way out
By Newsday
Apr. 18, 2024
Interest rates seen tumbling below 20%

RBZ deputy governor Innocent Matshe said several measures taken by the central bank early this month, including the launch of the new currency, would stabilise the economy.
By Mthandazo Nyoni
2h ago
Nyazema lands CBZ CEO post
By Blessed Ndlovu
2h ago
Invictus inks gas to power deal
By TAFADZWA MHLANGA
Apr. 24, 2024
Zimplow CEO resigns
By Business Reporter
Apr. 24, 2024
Zim exports uncompetitive: ZimTrade
By Melody Chikono
Apr. 24, 2024
'Legislation to propel SMEs funding plan'
By Business Reporter
Apr. 23, 2024
WestProp revenue in 38% jump
By Mthandazo Nyoni
Apr. 23, 2024
2030 upper-middle income vision under threat: Veritas
By Tatira Zwinoira
Apr. 23, 2024
RBZ promises SMEs financial injection
By Melody Chikono and BELINDA CHIROODZA
Apr. 23, 2024
.
Sport
.
Opinion
NewsDay cartoon 28 November, 2023 edition
NewsDay cartoon 28 November, 2023 edition
By The Watcher
Nov. 28, 2023
Govt urges unity among lithium miners
Currently there are around eight different lithium exploration and mining projects at different development stages.
By Mthandazo Nyoni
Jun. 1, 2023
Over 130 civilians killed by DR Congo rebels - UN
By BBC News
Dec. 8, 2022
Opaque Chinese deals: Mthuli taken to task
By admin
Aug. 29, 2022
Power outages, raw material shortages hit ART operations
By The NewsDay
Aug. 17, 2022
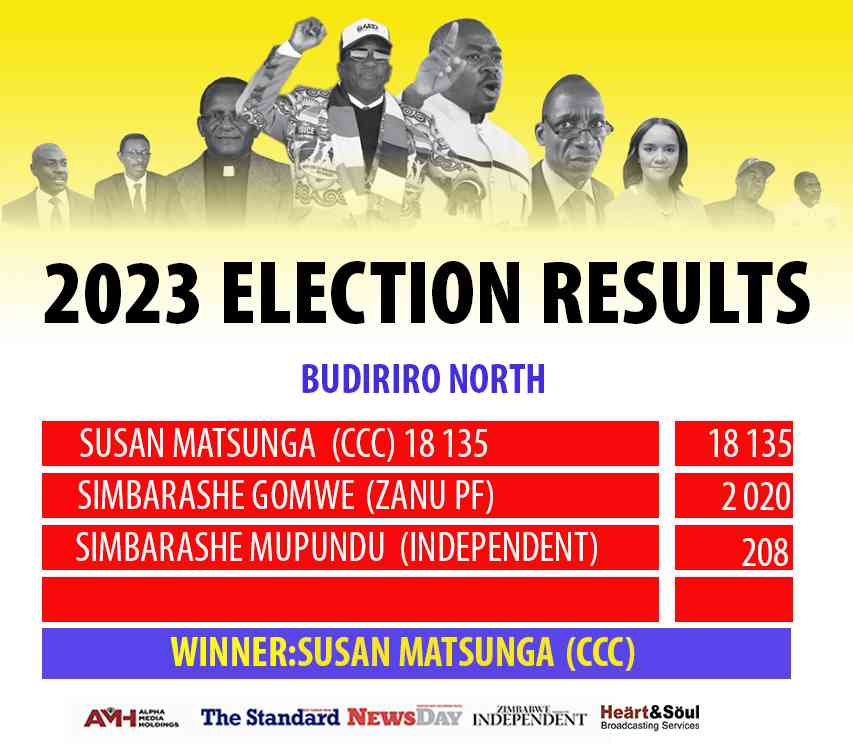
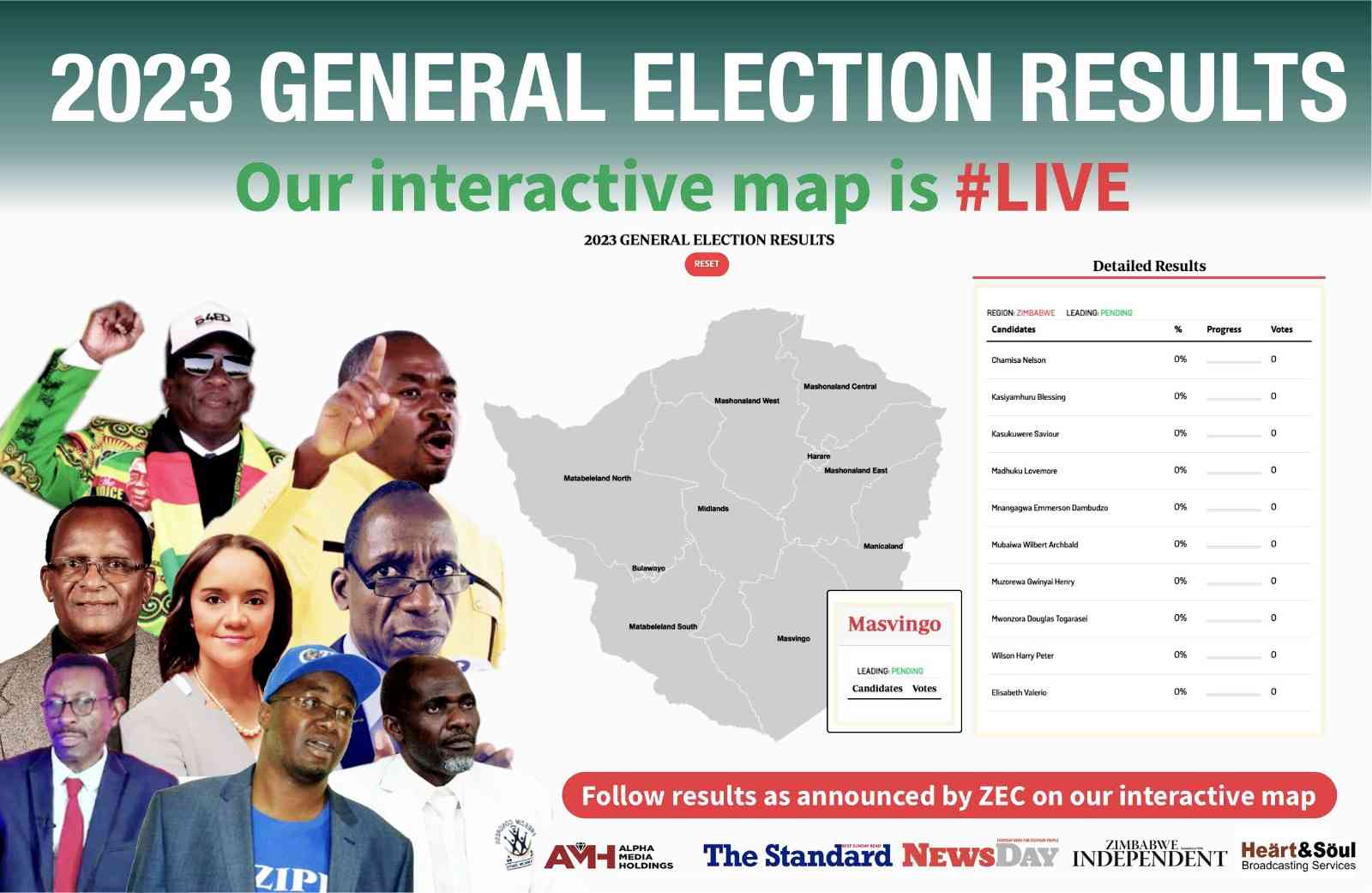
We’re unstoppable: CCC
By The NewsDay
Aug. 16, 2022
Umzingwane, Matobo main road ‘forgotten’
Matobo ward 15 councillor Dickson Moyo said the Old Gwanda road, which is major road passing through Umzingane and Matobo, had been neglected for more than five years.
By The NewsDay
Jul. 29, 2022
The existential crisis of Zim’s national identity
Throughout our rich history, we have fought against colonialism, struggled for independence, and yearned for a future defined by justice and equality.
By AMH Voices
2h ago
Wash boost for indigenous churches
By Style Reporter
20h ago
Mahachi pays tribute to late SA gospel icon
Mahachi and Ncwane collaborated on a 2015 hit single titled Ndinoda Jesu/Ngiyamuthanda uJesu, which marked the beginning of their connection.
By Style Reporter
Apr. 23, 2024
Richest Forex Traders in Tanzania
By The Standard
Apr. 22, 2024
Binga South MP, minister clash over boreholes
Cumanzala, however, said villagers in the constituency had dismissed the minister’s claims.
By Patricia Sibanda
2h ago
Councillor pleads for waste pickers
By Patricia Sibanda
Apr. 24, 2024
Food vendors overrun Byo streets after hours
By Innocent Magondo
Apr. 24, 2024
SA turns on heat on Zim smugglers
By Rex Mphisa
Apr. 24, 2024
De Souza banks on speed, agility.

Zimbabwe U20 rugby team head coach, Shaun De Souza is happy with the team’s preparations and looking forward to their tournament opener against Tunisia.
By AUSTIN KARONGA
Apr. 19, 2024